In the quest for a more youthful appearance, many individuals explore cosmetic procedures that can address the effects of aging. Two popular options are the parotid and facelift surgeries. These procedures, though distinct, are often sought together for comprehensive rejuvenation. In this article, we will delve into the world of parotid and facelift surgeries, understanding their significance, procedures, benefits, and potential risks.
1. Understanding the Parotid Glands
The parotid glands, located on either side of the face, are the largest of the salivary glands. These structures play a crucial role in producing saliva, aiding in the digestion process. Beyond their functional role, the parotid glands can also impact one’s appearance, especially as they age. Enlarged or sagging parotid glands can lead to a “jowl” effect, contributing to an aged and tired appearance.
2. The Facelift: An Overview
The facelift, also known as a rhytidectomy, is a cosmetic surgical procedure designed to address signs of aging in the face and neck. It involves tightening the facial muscles, removing excess skin, and repositioning tissues to create a smoother and more youthful appearance. While the facelift is highly effective in treating certain facial concerns, it may not specifically target the parotid glands.
3. Combining Parotid and Facelift Surgeries
For individuals seeking a comprehensive facial rejuvenation, the combination of parotid and facelift surgeries can be a powerful solution. By addressing both the sagging parotid glands and other facial aging concerns simultaneously, patients can achieve a more balanced and natural-looking result.
4. The Parotid Surgery Procedure
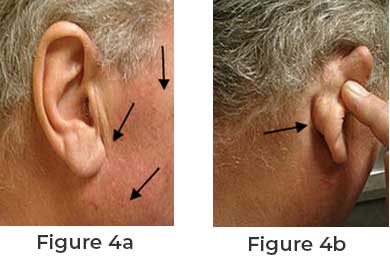
Parotid surgery, also known as parotidectomy, is a surgical procedure performed to remove all or part of the parotid gland. This surgery is usually recommended when there are issues such as tumors, infections, or excessive enlargement of the gland. During the procedure, the surgeon makes an incision in front of the ear and carefully removes the affected gland.
5. The Facelift Surgery Procedure
The facelift surgery is typically performed under general anesthesia. The surgeon begins by making incisions around the hairline and behind the ears. Through these incisions, the facial muscles are tightened, excess fat is removed or repositioned, and the skin is draped back into place. The incisions are then closed, leaving the patient with a rejuvenated and youthful appearance.
6. Benefits of Parotid and Facelift Surgeries
• Comprehensive Facial Rejuvenation: The combination of both surgeries addresses various signs of aging, providing more balanced results.
• Natural-Looking Outcome: When performed by an experienced surgeon, the results are subtle and natural-looking, enhancing the patient’s appearance without an artificial look.
• Boost in Self-Confidence: Many patients report increased self-esteem and confidence after undergoing these procedures.
7. Potential Risks and Considerations
As with any surgical procedure, both parotid and facelift surgeries carry certain risks. These may include infection, scarring, bleeding, nerve damage, and unfavorable aesthetic outcomes. It is essential for patients to thoroughly discuss the risks and potential complications with their surgeon before making a decision.
8. Post-Operative Care and Recovery
After undergoing parotid and facelift surgeries, patients can expect some swelling, bruising, and discomfort. Following the surgeon’s post-operative instructions is vital for a smooth and successful recovery. Rest, proper wound care, and avoiding strenuous activities are essential during this period.
9. Are You a Good Candidate?
Not everyone is a suitable candidate for parotid and facelift surgeries. Ideal candidates are generally in good health, have realistic expectations, and wish to address specific facial aging concerns. A consultation with a qualified surgeon is crucial to determine if these procedures are appropriate for an individual’s unique needs.