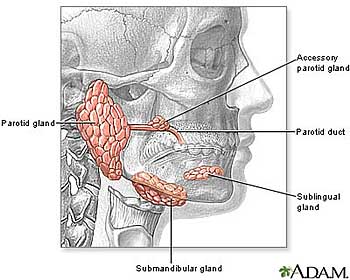
Facial nerve cancer, also known as facial nerve schwannoma or facial nerve neuroma, is a rare condition characterized by the growth of tumors on or around the facial nerve. The facial nerve, also called the seventh cranial nerve, is responsible for controlling the muscles of facial expression and transmitting taste sensations from the front two-thirds of the tongue. When cancer affects this nerve, it can lead to various symptoms that can impact facial function and quality of life. Understanding the symptoms and treatment options for facial nerve cancer is essential for early detection and effective management of the condition.
Symptoms of Facial Nerve Cancer
Facial weakness or paralysis is the first and one of the common symptoms. Patients will notice the development of weakness or paralysis on one side of the face. This can manifest as drooping of the mouth, inability to close the eye fully, and difficulty making facial expressions.
Facial Pain or Numbness
Some individuals with facial nerve cancer may experience pain, tingling, or numbness in the affected area. This can be due to compression of the nerve by the tumor or irritation of nearby structures.
Hearing Loss or Tinnitus
Tumors affecting the facial nerve may also affect the nearby auditory nerve, leading to hearing loss or ringing in the ears (tinnitus). This can occur if the tumor grows large enough to press on the structures of the inner ear.
Changes in Taste
Since the facial nerve also plays a role in transmitting taste sensations from the tongue, individuals with facial nerve cancer may experience alterations in taste perception or loss of taste on the affected side of the tongue.
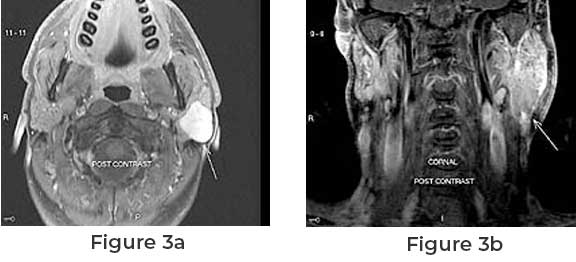
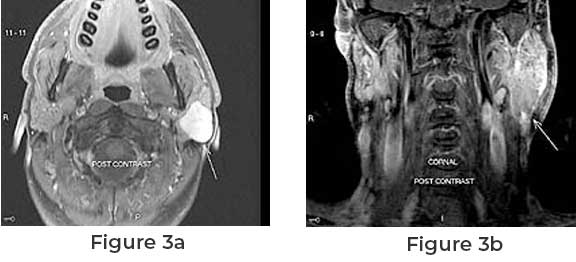
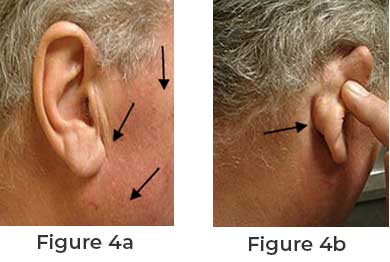
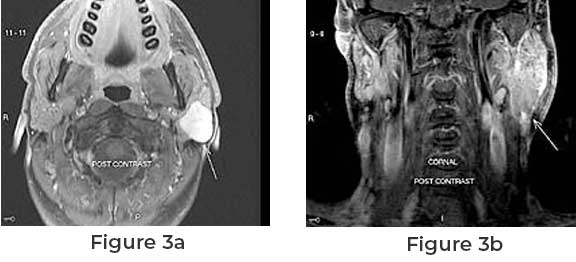
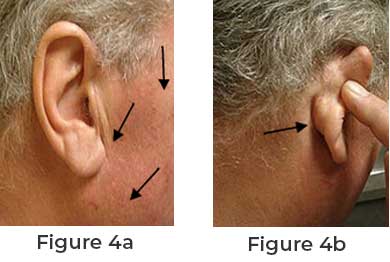
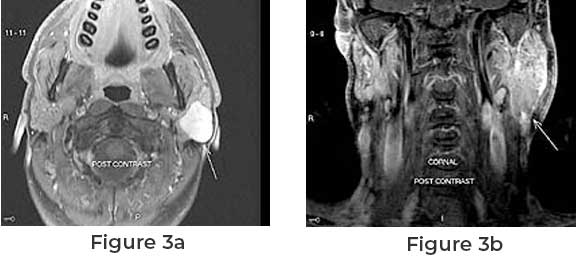
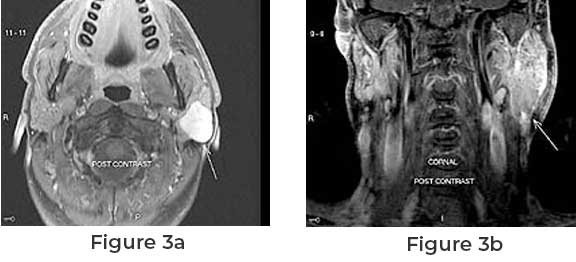
Facial Swelling or Mass
As the tumor grows, it may cause swelling or a palpable mass in the affected area, typically near the ear or along the course of the facial nerve.
Treatment Options for Facial Nerve Cancer Surgical removal of the tumor is often the primary treatment for facial nerve cancer. The goal of surgery is to completely excise the tumor while preserving as much of the facial nerve functions as possible. In some cases, partial or total removal of the affected facial nerve may be necessary, which can result in permanent facial weakness or paralysis.