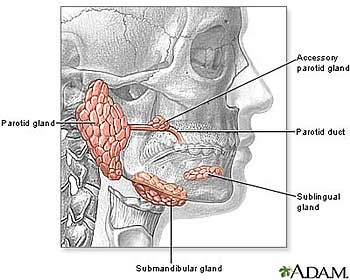
Salivary gland tumors, though relatively rare, can significantly impact health and quality of life. These tumors can arise in any of the major salivary glands—parotid, submandibular, or sublingual—as well as in minor glands scattered throughout the mouth and throat.
Types of Salivary Gland Tumors
There are several types of salivary gland tumor, with the most common being pleomorphic adenomas, also known as benign mixed tumors. These usually occur in the parotid gland and are generally not life-threatening, although they may require surgical removal to prevent complications. On the other hand, malignant tumors such as mucoepidermoid carcinoma and adenoid cystic carcinoma are more serious and can metastasize if not treated promptly.
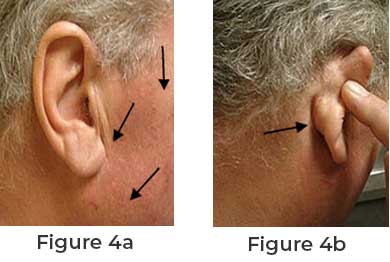
Symptoms to Watch For
Common symptoms of salivary gland tumors include a noticeable lump or swelling near the jaw, persistent pain, difficulty swallowing, or changes in the taste of food. Some individuals may also experience facial numbness or weakness, which should prompt immediate medical evaluation.
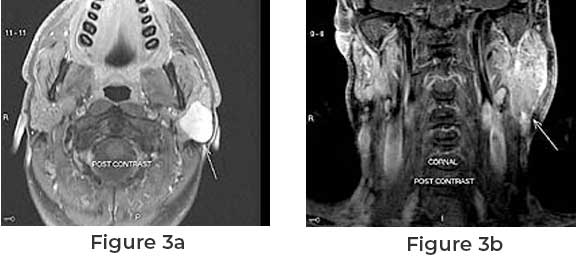
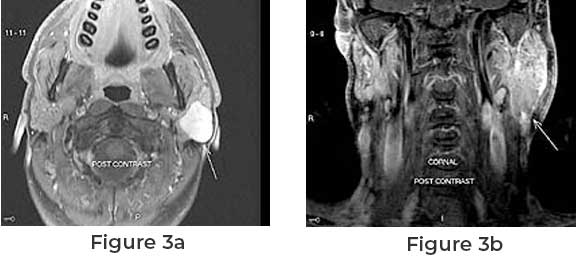
Diagnosis and Treatment
Diagnosis typically involves imaging tests like MRI or CT scans, along with a biopsy to determine the nature of the tumor. Treatment options vary depending on the tumor’s type, size, and location. For benign tumors, surgical excision is often sufficient, while malignant tumors may require more extensive surgery, radiation therapy, or chemotherapy.
Prognosis and Outlook
The prognosis for salivary gland tumors varies widely. Benign tumors generally have a favorable outcome, while the prognosis for malignant tumors depends on factors such as stage and overall health. Early detection and treatment are crucial for the best outcomes.
If you experience any concerning symptoms, consult a healthcare professional for a thorough evaluation. Awareness and timely intervention are key to managing salivary gland tumors effectively.